Back Pain
The spine is a strong and flexible structure connecting the skull to the pelvis. It comprises of 33 blocks of bone called vertebra. The spine is separated into 5 distinct areas including:
- The neck (cervical spine comprising 7 vertebra – naturally forming a gentle lordotic curve)
- Mid back (thoracic spine comprising 12 vertebra – naturally forming a gentle kyphotic curve)
- Lower back (lumbar spine comprising 5 vertebrae – naturally forming a gentle lordotic curve)
- The sacrum (comprising 5 vertebra)
- The coccyx (tail bone comprising between 3-5 vertebra).
The vertebrae within the neck, mid back and lumbar spine are separated by shock absorbing structures called intervertebral discs. The sacral and coccyx vertebra are fused and do not have discs.
The spine is an amazing structure affording excellent mobility/flexibility. It also provides protection to important neurological structures such as the spinal cord which is contained within a natural tunnel of bone within the spine called the spinal canal. Due to the amount of nervous tissue around the spine it can be a pain sensitive area.
Occasionally the spine can curve from side to side as well as the normal front to back curves (lordosis and kyphosis). Side to side curvature is called scoliosis and in mild degrees is quite normal and harmless but if it is severe of worsening over time this may need further investigation.
What are the common causes of back pain?
Most people suffer from lower back problems (low back pain or lower back related leg pain) at some point in their lives. They are very common. The majority of the time it doesn’t mean actual damage to your back.
There are different anatomical structures thought to cause spinal pain including the intervertebral discs, facet joints, nerves, surrounding soft tissues including muscles, tendons, ligaments and other connecting joints. Most back pain, however, can start for no obvious reason, this can be very frustrating.
The truth is that despite advances in imaging techniques it is often very difficult, if not impossible, for us to be able to find the exact cause or structure for most spinal pain. This is why an x-ray or an MRI scans are not needed in the management of spinal pain.
Most people with back pain need to keep moving and the pain will settle with time. Please click on the information below to find out how to manage your pain.
Common conditions of the Back
See below for the common signs and symptoms with a link to the MSK Matters page on how best to manage it.


Lower back pain
- Can be a sudden onset or develop over time
- Pain can be sharp, shooting, dull ache, hot or burning
- Pain can be anywhere on the back, central or more on one side
- Occasionally there may be some pins and needles or numbness felt
- Can disturb sleep
Click here for more information on lower back pain
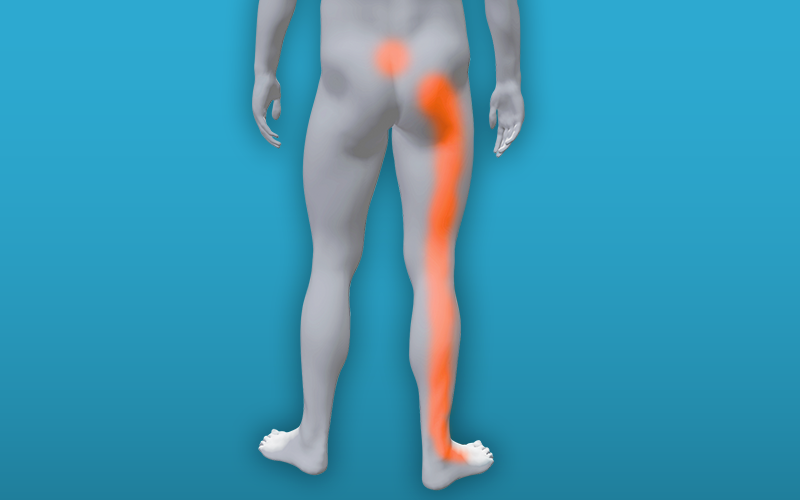
Low back related leg pain – Sciatica
- Pain and symptoms maybe in your bottom, back of your leg, foot and toes
- You may have some back pain, often this is less painful than the leg
- Pain maybe stabbing, burning or shooting
- You may feel tingling (pins and needles)
- You may have some numbness
- You may have some weakness in the leg
- It may disturb your sleep
Click here for more information on low back related leg pain – Sciatica
Lumbar Spinal Stenosis
- Pain and symptoms maybe in your bottom, back of your leg, foot and toes. Pain can be in one leg or both
- You may have some back pain
- Symptoms often occur in standing and walking
- Pain maybe stabbing, burning or shooting
- You may feel tingling (pins and needles) into your legs
- Discomfort, numbness, weakness or feelings of unsteadiness in the legs
- It may disturb your sleep
- Some people will also experience pain in lying and leg cramps, particularly at night
- Symptoms are often reduced if sitting or leaning forward
Click here for more information on Lumbar Spinal Stenosis
Is your pain coming from somewhere else?
All the anatomical structures named above can cause pain that is experienced in a different location to actual site of the irritable structure. For example, it is possible for the lower back to refer pain through to the groin and to the outer thigh amongst other sites.
At every level of the neck, mid back and lumbar spine and sacrum there are a pair of nerve roots which branch off from the spinal cord and exit the spine to serve certain areas of the limbs or trunk with skin sensation and muscle power as well as other functions. As a rough guide, nerves which exit the neck will serve the arm / hand, nerves exiting the mid back will serve the trunk and nerves exiting the lumbar spine will serve the legs / feet. These nerves follow a pattern so when a nerve becomes irritated we can usually identifying which spinal level may be causing problems during clinical assessment. The classic example of an irritated nerve in the lower back is sciatica which refers pain into the leg – sometimes as far as the foot.
When to seek medical advice
Many patients have a combination of back pain, leg pain, leg numbness and weakness. These symptoms can be distressing for you but don’t necessarily require emergency medical attention.
A rare but serious back condition, Cauda Equina Syndrome, can lead to permanent damage or disability and will need to be seen by an Emergency Specialist Spinal Team.
Please seek urgent medical advice and attend the Emergency Department if you experience any of the Cauda Equina Syndrome warning signs below:
- Loss of feeling/ pins and needles between inner thighs or genitals
- Numbness in or around your back passage or buttocks
- Altered feeling when using toilet paper to wipe yourself
- Increasing difficulty when you try to urinate
- Increasing difficulty when you try to stop or control your flow of urine
- Loss of sensation when you pass urine
- Leaking urine or recent need to use pads
- Not knowing when your bladder is either full or empty
- Inability to stop a bowel movement or leaking
- Loss of sensation when you pass a bowel movement
- Change in ability to achieve an erection or ejaculate
- Loss of sensation in genitals during sexual intercourse
The majority of musculoskeletal conditions get better within six to eight weeks although sometimes they can persist for longer but this doesn’t mean there is something seriously wrong.
However, rarely, musculoskeletal symptoms can be caused by something more serious and it is important for you to know when to seek advice. We would advise if you experience any of the following you should seek the advice of you GP.
- the pain you are experiencing is getting worse rather than better despite following the self-management guidance above for the condition in the time frame expected
- symptoms have not been significantly helped by a trial of medication as expected
- you feel unwell and suffer symptom such as fever, night sweats or weight loss
- you experience pain at night, possibly worse than during the day that prevents you from sleeping due to increasing pain and/or difficulty lying flat.
- you experience a change in your ability to walk including balance problems or weakness/heaviness in your legs
- you develop a hot and swollen joint for no apparent reason
- early morning stiffness, lasting for longer than 30 minutes
